This year, over 53,000 Americans are estimated to lose their lives to colorectal cancer. Despite being the second leading cause of cancer deaths in the United States, early detection can lead to a cure. Detecting a tumor as early as possible allows for prompt treatment, increasing the chances of survival.
As a gastroenterologist, I treat patients from various backgrounds who are facing a growing number of obstacles to accessing timely care. Insurance barriers often delay coverage determinations or result in outright denials.
With the concerning increase in colorectal cancer diagnoses among Americans under 50, it is crucial for individuals to be aware of their cancer risk and the recommended screening timing.
Here are some common questions that patients frequently ask myself and other gastroenterologists about colorectal cancer:
- What is my risk of developing colorectal cancer?
Colorectal cancer can affect anyone regardless of age, but certain individuals may have a higher susceptibility to the disease.
Those with a family history of colorectal cancer or a personal history of polyps, which are abnormal growths in the colon or rectum, are at a greater risk.
Moreover, individuals with inflammatory bowel diseases such as Crohn’s or ulcerative colitis have an increased likelihood of developing colorectal cancer. This is due to the chronic inflammation associated with these conditions, which can encourage the formation of abnormal growths.
Race and ethnicity can impact the risk of developing colon cancer. Black and Indigenous Americans have a significantly higher likelihood of both developing and dying from colorectal cancer. While genetics do play a role, many environmental factors contribute to the risk, such as income level, access to healthcare, and the availability of nutritious food options in the community.
Unhealthy lifestyle choices, such as smoking, lack of exercise, and a poor diet, can also increase the risk of colon cancer. Research has shown that certain chemicals released by red meat can cause inflammation, while a diet rich in fiber and vegetables can help reduce inflammation. Additionally, a sedentary lifestyle and smoking can lead to genetic changes in colon cells that are harmful.
When it comes to screening for colon cancer, there are several options available.
Colorectal cancer often shows no symptoms until it reaches an advanced stage, underscoring the importance of early and regular screening.
To address the rising incidence of colorectal cancer in younger adults, the U.S. Preventive Services Task Force now advises regular screenings to begin at age 45, down from 50 in 2021. People at higher risk may need to start screening earlier and undergo more frequent tests.
There are different screening options available, and your healthcare provider can suggest the most appropriate procedures based on your individual risk factors.
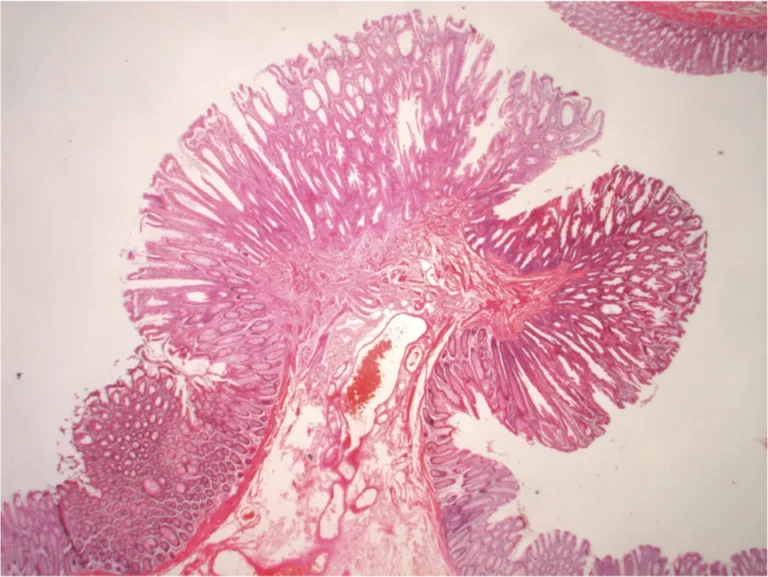
A popular choice for many individuals is to undergo a colonoscopy, a screening test that not only detects but also prevents cancer by eliminating potentially cancerous polyps. This procedure utilizes a flexible tube equipped with a light and camera to visually examine the colon for any signs of cancer, abnormalities in the colon lining, or the presence of growths like polyps. Ultimately, colonoscopy screening plays a crucial role in reducing the occurrence and death rates associated with colorectal cancer.
Additionally, alternative screening methods include noninvasive stool testing, imaging scans, as well as a combination of endoscopic visualization and stool-based testing.
Your doctor can assist you in selecting a test that is in line with your preferences, values, and risk factors. Recommended screening methods for individuals with an average risk of colon cancer include a colonoscopy every 10 years, stool-based testing every one to three years, or CT scans every five years for those unable to undergo a colonoscopy initially. In the case of a positive result from these alternative approaches, a colonoscopy should be conducted.
By undergoing regular screening, one in three deaths caused by colorectal cancer can be prevented.
Why is my health insurance not covering the cost of my colonoscopy?
Although colorectal cancer screening is provided free of charge as a preventive service under the Affordable Care Act, some insurers are creating barriers to accessing care.
Take, for instance, the case of Blue Cross Blue Shield of Massachusetts. They initially proposed a policy in 2024 that would have classified the use of anesthesia in crucial procedures like endoscopies and colonoscopies as medically unnecessary. This would have forced patients to pay out of their own pockets for anesthesia during colorectal cancer screenings, potentially creating significant financial barriers. It was only after strong opposition from doctors and patients that the insurance company reversed its decision.
Another concerning trend is the increased use of prior authorization by health insurers. This is a process used to determine whether they will cover the costs of a medical procedure, service, or medication. However, insurers can sometimes delay or deny coverage for medically necessary care recommended by physicians and medical guidelines. They may consider certain healthcare services unnecessary for a patient or too costly to cover.
In 2023, UnitedHealthcare proposed a policy that would have made it mandatory for the 27 million individuals under their plan to obtain insurance approval before undergoing diagnostic or follow-up colonoscopies. However, due to protests from physicians and patients, the insurer decided to put the policy on hold.
Additionally, UnitedHealthcare is planning to introduce a program in 2024 that may involve prior authorization for colonoscopies. However, the insurer has provided limited information regarding the rationale behind these requirements, which services would necessitate prior authorization, and how it plans to ensure that patients are not subjected to unnecessary delays or denials.
To reduce your risk of colorectal cancer, it is advisable to consider getting screened if you haven’t already. It is recommended that you discuss this with your doctor’s office and check with your insurance company to understand what will be covered prior to undergoing the procedure. If you are 45 years of age or older, a colonoscopy can be an effective screening method to detect and prevent colorectal cancer.
Taking proactive measures in terms of diet and lifestyle can significantly lower the chances of developing colon cancer in younger adults. It is important to be mindful of individual risk factors and seek medical help if any symptoms, such as changes in bowel movements, rectal bleeding, abdominal pain, or unexplained weight loss, occur. By doing so, you can have a productive conversation with your healthcare provider about available screening options.
If you have already undergone a colonoscopy and had polyps removed, it is crucial to stay informed about when your follow-up colonoscopy is due. This simple step could potentially save your life.
