After nearly 20 years since its introduction, research has shown that individuals who received the HPV vaccine have a significantly lower risk of developing HPV-related cancers later in life.
According to the World Health Organization, HPV is a widespread viral infection that leads to approximately 690,000 cancer cases annually worldwide. This virus targets specific tissues, making patients more susceptible to developing various types of cancers, such as cervical, anal, and head and neck cancer.
Initially marketed as a cervical cancer prevention tool for young women, the HPV vaccine was approved in 2006. Over time, it has been updated to offer protection against additional strains of HPV and is now recommended for boys as well. By expanding its usage, the vaccine aims to reduce the risk of anal and head and neck cancers. Currently, the vaccine is recommended for children aged 11 or 12, unvaccinated adults until the age of 26, and can be recommended by healthcare professionals up to the age of 45.
Experts are now observing early indications of the positive effects of cancer prevention. A recent report from Scotland in early 2024 revealed that there were no cases of cervical cancer among individuals who received the HPV vaccine at the age of 12 or 13. This study, which examined hundreds of thousands of patients participating in a routine vaccination program with a high uptake rate of 80%, is one of the first to analyze the impact of HPV vaccination at a population level.
Furthermore, the benefits of HPV vaccination extend beyond cervical cancer. In high-income countries like the United States, head and neck cancer has now surpassed cervical cancer as the primary HPV-related cancer. This highlights the broader impact and significance of HPV vaccination in reducing the risk of various types of cancer.
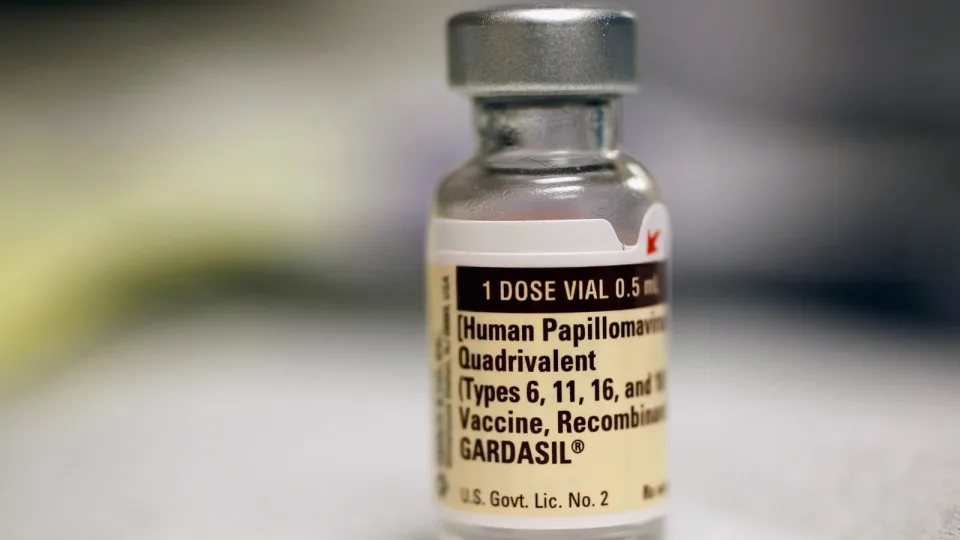
(Photo: A bottle of the Human Papillomavirus vaccination is seen at the University of Miami Miller School of Medicine in Miami, FL, Sep. 21, 2011. – Joe Raedle/Getty Images)
Preliminary reports presented at the May 2024 American Society of Clinical Oncology (ASCO) conference revealed a promising 56% decrease in the risk of HPV-associated head and neck cancer among vaccinated men.

Dr. Michelle Chen, an Assistant Professor at Stanford University and a head and neck cancer surgeon, expressed excitement about the study results, stating that they align with expectations that HPV vaccination will significantly reduce the occurrence of HPV-related head and neck cancer.
Dr. Erich Sturgis, a professor at the Baylor Department of Otolaryngology-Head & Neck Surgery and an expert in HPV-positive oropharyngeal cancers, emphasized that the full benefits of the HPV vaccine are likely to be realized in the coming decades, based on available data.
According to Sturgis, it may take a few more decades before we see the full impact of the HPV vaccine, as the majority of those affected by HPV-related cancers are in their 50s, 60s, and 70s. On a positive note, there has been an increase in people getting vaccinated, as the vaccines are proven to be safe, effective, and provide long-lasting protection.
A recent study presented at the 2024 ASCO conference revealed that the uptake of the HPV vaccine in the United States has steadily improved from 23.3% in 2011 to 43% in 2020. Chen stated that overall, we are moving in the right direction, particularly with regards to increasing vaccination rates among males, who have traditionally lagged behind females.
Nevertheless, doctors continue to emphasize the importance of vaccination for all eligible individuals. As of 2022, the percentage of teenagers who are up-to-date on their HPV vaccination has plateaued at around 63%, according to the Centers for Disease Control and Prevention.
According to Chen, our progress towards the Healthy People 2030 target of achieving an 80% HPV vaccination rate is significantly lagging.